All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know ALL.
The all Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the all Hub cannot guarantee the accuracy of translated content. The all and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The ALL Hub is an independent medical education platform, sponsored by Amgen, Autolus, Jazz Pharmaceuticals, and Pfizer and supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View ALL content recommended for you
Impact of socioeconomic factors on survival outcomes in adult ALL: Key updates from ASH 2023
Do you know... In the multivariate analysis of adult patients with acute lymphoblastic leukemia treated at the University of Chicago, which of the following factors was significantly associated with overall survival (OS)?
While survival outcomes have considerably improved for adult patients with acute lymphoblastic leukemia (ALL), there are persistent disparities by race/ethnicity and socioeconomic status: Hispanic and Black patients, those with a lower socioeconomic status, being uninsured, and a lack of access to care have been associated with poor outcomes.1–3 As such, there is a need for novel approaches and therapies to address these disparities.1
Here, we summarize four presentations describing key trials investigating the impact of socioeconomic factors on survival outcomes in adult patients with ALL, presented at the 65th American Society of Hematology (ASH) Annual Meeting and Exposition.
Impact of social determinants of health on brexucabtagene autoleucel outcomes: ROCCA study1
Results from the ongoing, retrospective, multicenter Real-World Outcomes Collaborative of CAR-T in Adult ALL (ROCCA) study evaluating the impact of social determinants of health on overall survival (OS) and progression-free survival (PFS) outcomes in adults with B-cell ALL receiving commercial brexucabtagene autoleucel (brexu-cel) between 2021 and 2023 were presented by O’Connor.
The social deprivation index (SDI), composed of seven demographic characteristics (percentage of poverty, <12 years of education, single-parent household, rented housing, overcrowding, households without cars, and non-employment), was used to quantify socioeconomic variation in health outcomes at the zip-code level; higher SDI indicated greater social disadvantage. Patients were subdivided into high (66–100% percentile), medium-high, low-medium, and low SDI (0–25% percentile).
Results
A total of 152 patients with at least 3 months of follow-up were included in the analysis. The population was ethnically diverse, included mainly older patients, and 26% had a high SDI. The majority of patients had received a median of four prior lines of therapy, had primarily public (49%) and private (42%) health insurance, were referred from private/community-based practices (46%), and lived within 50 miles of the CAR T-cell therapy center (62%). No patients were uninsured. The median follow-up was 12.3 months.
In the univariate analyses, there was no difference in PFS between Hispanic and non-Hispanic White patients and in patients with high vs low SDI. Multivariate analyses revealed no significant difference in PFS by race, sex, distance to CAR T-cell therapy site, insurance type, referral source, lines of therapy, and age at CAR T-cell infusion.
Presenter’s conclusion
Despite the limitations of sample size and selection bias, this real-world analysis reported similar PFS outcomes by race and across different social determinants of health insurance type, referral source, distance to CAR T-cell center, and SDI in adult patients receiving brexu-cel. These data suggest that improving access to brexu-cel treatment may improve overall outcomes for historically disadvantaged populations with relapsed/refractory B-cell ALL.
Impact of socioeconomic and biological factors2
Data from a single-center, retrospective study investigating the impact of socioeconomic and biological factors on outcomes in adult patients with ALL treated at the University of Chicago between 2010 and 2022 were presented by Johnston. Analyses were stratified by age: adolescent and young adults (AYA; 18-40 years) and older adults (≥ 40 years). Outcomes were compared with the national Surveillance, Epidemiology, and End Results (SEER) data.
Results
A total of 221 patients were included in the analysis, comprising non-Hispanic White (59%), Hispanic (22%), and non-Hispanic Black patients (15%).
At the University of Chicago, there was no significant difference in the OS by race and median household income when stratified by AYA and older patients; however, among the SEER cohort, non-Hispanic White AYA patients had a significantly better OS when compared with Hispanic and non-Hispanic Black patients; and older patients with a higher median household income had a better OS than those with a lower median household income.
The multivariate analysis showed a significant difference in OS based on age and body mass index, but there was no difference in OS based on race and income.
Presenter’s conclusion
Compared with the SEER data, race/ethnicity and socioeconomic factors did not influence OS outcomes in patients treated at the University of Chicago. Treatment at this dedicated AYA clinic offers resources to support patients, as well as clinical trial options. With this institution being located in a historically Black and low-income neighbourhood, it plays a crucial role in addressing the socioeconomic disparities in ALL care. Further studies looking at the impact of obesity on outcomes in ALL are needed.
Impact of socioeconomic disadvantage on racial and ethnic disparities3
Using data from SEER, the association of socioeconomic disadvantage and long-term survival outcomes in AYA patients aged 15−39 diagnosed with ALL between January 1, 2005 and December 31, 2019 was investigated; these results were presented by Knight. The area deprivation index (ADI) was used as a measure of socioeconomic disadvantage, with a high ADI indicating significant socioeconomic disadvantage and low ADI indicating less disadvantage. The ADI quartiles were assigned by decade, and the 2009 and 2019 ADI scores were used based on patient diagnosis year. Cause-specific and observed survival were calculated over 5-year periods.
Results
A total of 4,382 patients were included in the analysis; they had an observed survival of 60.6%.
- Among patients diagnosed during 2005−2009, the 48-month and 60-month cause-specific and observed survivals were significantly higher in those living in a county with an ADI value of 1 vs those with an ADI value of 4.
- For patients diagnosed during 2010−2014, there were no significant differences in the cause-specific or observed survival by ADI quartile.
- For patients diagnosed during 2015−2019, the 36-month and 48-month cause-specific survival was significantly higher in those living in a county with an ADI value of 1 than those living in a county with an ADI value of 4 (p < 0.05).
- The 12-, 24-,36- and 48-month observed survivals were also significantly higher for those with ADI value of 1 vs 4 for those who were diagnosed during 2015−2019 (Figure 1).
- There was no statistically significant difference in the cause-specific and observed survivals between states that expanded Medicaid versus those that did not.
Figure 1. Observed survival rates by ADI quartile for patients diagnosed during 2015−2019*
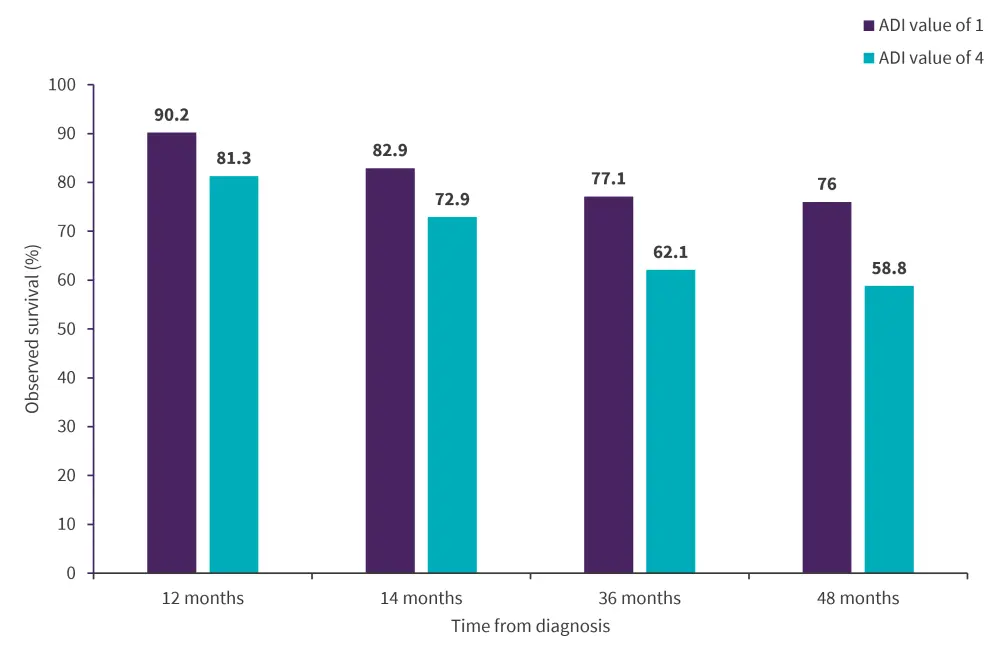
*Adapted from Knight.3
Presenter’s conclusion
Socioeconomic disadvantage was significantly associated with worse long-term survival outcomes in AYA patients with ALL. These disparities persist over time despite treatment advances and public policy changes; thus, there is an urgent need for interventional approaches for this vulnerable patient population.
Racial and ethnic disparities among AYA patients4
Data from the retrospective cohort study using the Nationwide Inpatient Sample to assess the racial and ethnic disparities among AYA patients aged 15–39 years with ALL from January 1, 2011 to December 31, 2020 was reported by Lopez. Adjusted survey logistic regression analyses were used to assess the association between race/ethnicity and inpatient mortality, and joinpoint regression analyses was used to assess inpatient death among ALL hospitalizations by race/ethnicity.
Results
There were 138,923 ALL-related hospital encounters among AYA patients: 73.1% in patients aged ≥30 years and 26.9% in patients aged 30−39 years. In this population:
- Non-Hispanic Blacks had nearly twice the odds of inpatient mortality compared with non-Hispanic White patients (odds ratio, 1.75; 95% CI, 1.34–2.29; p < 0.01);
- Hispanic patients had an increased likelihood of inpatient mortality compared with non-Hispanic White patients (odds ratio, 1.32; 95% CI, 1.08–1.61; p = 0.01); though the inpatient mortality rate improved over time;
- The rate of inpatient mortality in non-Hispanic Black patients increased over the 10-year study period; and
- The lowest rate of inpatient mortality, both at the start and at the end of the study period, was seen in non-Hispanic White patients.
Presenter’s conclusion
This study reported racial and ethnic disparities in survival outcomes among the AYA population, with worse outcomes observed in non-Hispanic Black patients with ALL. As such, there is a need to better understand the disparities that impact AYA populations, as they are particularly vulnerable to social factors impacting their care.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content





