All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know ALL.
The all Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the all Hub cannot guarantee the accuracy of translated content. The all and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The ALL Hub is an independent medical education platform, sponsored by Amgen, Autolus, Jazz Pharmaceuticals, and Pfizer and supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View ALL content recommended for you
Patient and physician perceptions of palliative care during transplant
Do you know... According to a recent study by Melody et al., 28% of patients reported having “good” or “excellent” knowledge of palliative care before a palliative care consultation. What percentage of patients reported having “good” or “excellent” knowledge after the consultation?
Definitions of palliative care can vary, and the term is often subject to stigma due to associations with hospice and end-of-life care. In the context of patients undergoing hematopoietic stem cell transplantation (HSCT), palliative care can help patients to manage their symptoms and allow for advance care planning. However, perceptions of what palliative care is can vary between patients and physicians.
Here, we summarize two studies from the perspective of patient’s experiences with palliative care; one presented as a poster at the 2022 Society of Hematologic Oncology (SOHO) Annual Meeting by Melody et al.1 and one published by Gemmell et al.2 In addition, we summarize a study by Santivasi et al.,3 which focusses on physician perspectives of palliative care.
Patient perceptions
In the study by Melody et al.,1 32 patients who were undergoing evaluation for allogeneic HSCT were also referred for a palliative care consultation and asked to fill out a pre- and post-visit questionnaire. Results from two questions in this questionnaire are shown in Figure 1 and Figure 2. These figures highlight changes in patient knowledge and opinion of palliative care after a consultation.
Figure 1. Patient knowledge of palliative care pre- and post-consultation*
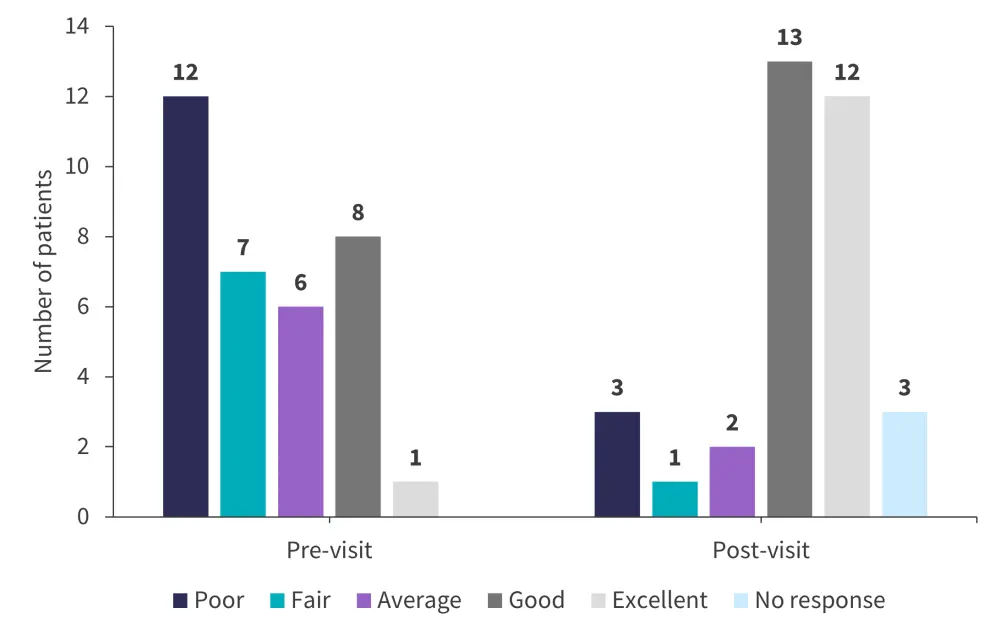
*Data from Melody, et al.1
Figure 2. Patient likelihood of continuing to utilize palliative care during transplant pre- and post-consultation*
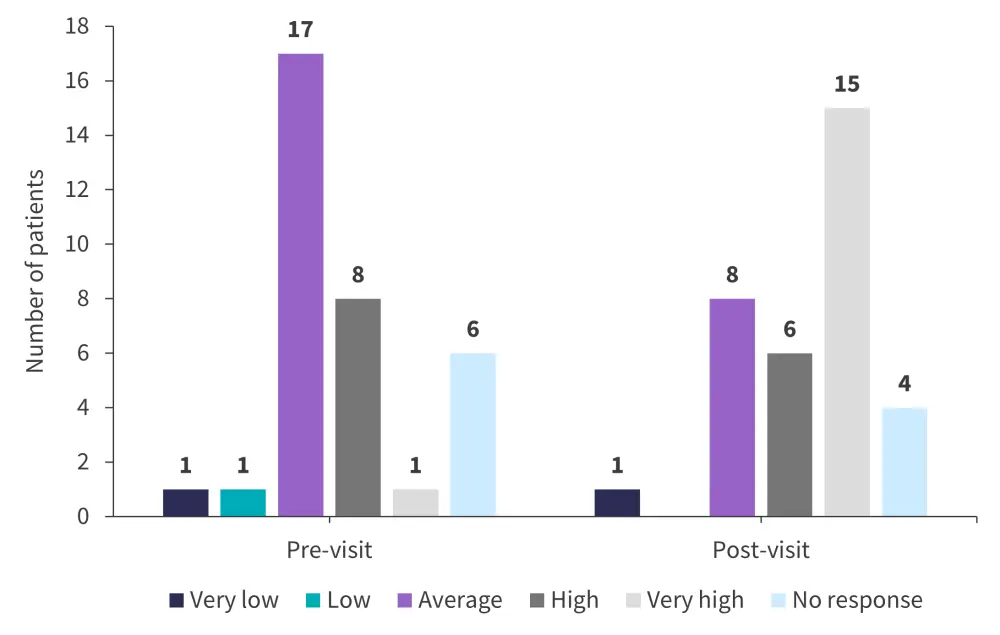
*Data from Melody, et al.1
In the study by Gemmell et al.,2 12 patients were interviewed, and four patients took part in a focus group (used to survey patients pre- and post-transplant). These were semi-structured and used the idea of themes to identify patient thoughts about palliative care, which are illustrated in Figure 3. Physician knowledge of patient thoughts about palliative care and what they require from their care could potentially improve communication between patients and physicians and increase uptake of palliative care. It is important to note that all 12 patients interviewed had no experience with palliative care, and two of the patients in the focus group had direct experience with palliative care during transplant.
Figure 3. Patient thoughts about five themes related to palliative care*
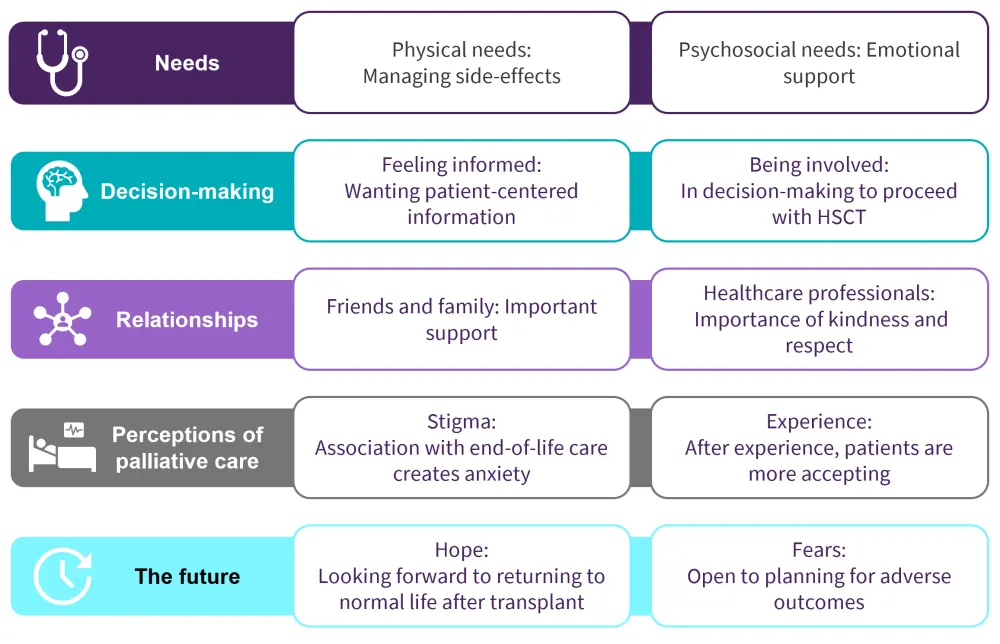
HCP, healthcare professional; HSCT, hematopoietic stem cell transplantation; PC, palliative care.
*Data from Gemmell, et al.2
Physician perceptions
In the study by Santivasi et al.,3 1,000 palliative care physicians were emailed a survey about comfort discussing prognosis with patients, palliative care, and relationships with hematologists. The response rate for the survey was 55.5%. Figure 4 and Figure 5 illustrate some results from the survey, focused on prognosis discussion and the factors that can influence a patient receiving a palliative care consultation. Overall, physicians reported feeling less comfortable in providing symptom management, discussing prognosis, and understanding disease trajectory for patients undergoing HSCT compared to patients with leukemia, lymphoma, or multiple myeloma.
Figure 4. Factors that influence physician comfort and discomfort in discussing prognosis with patients*
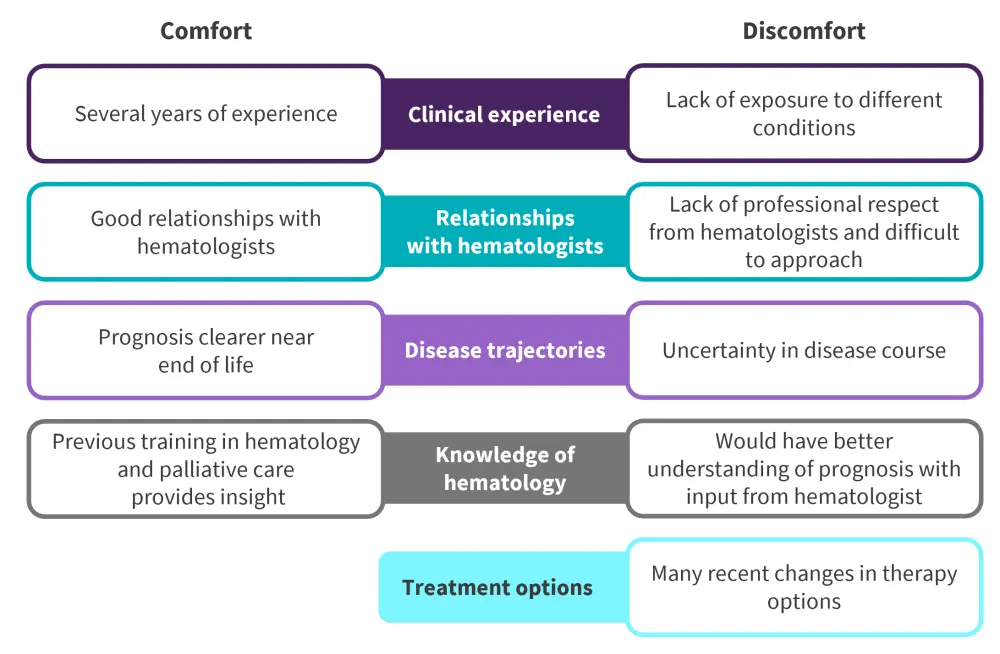
*Adapted from Santivasi, et al.3
Figure 5. Physicians’ responses to factors that influence a patient’s likelihood of receiving a palliative care consultation*
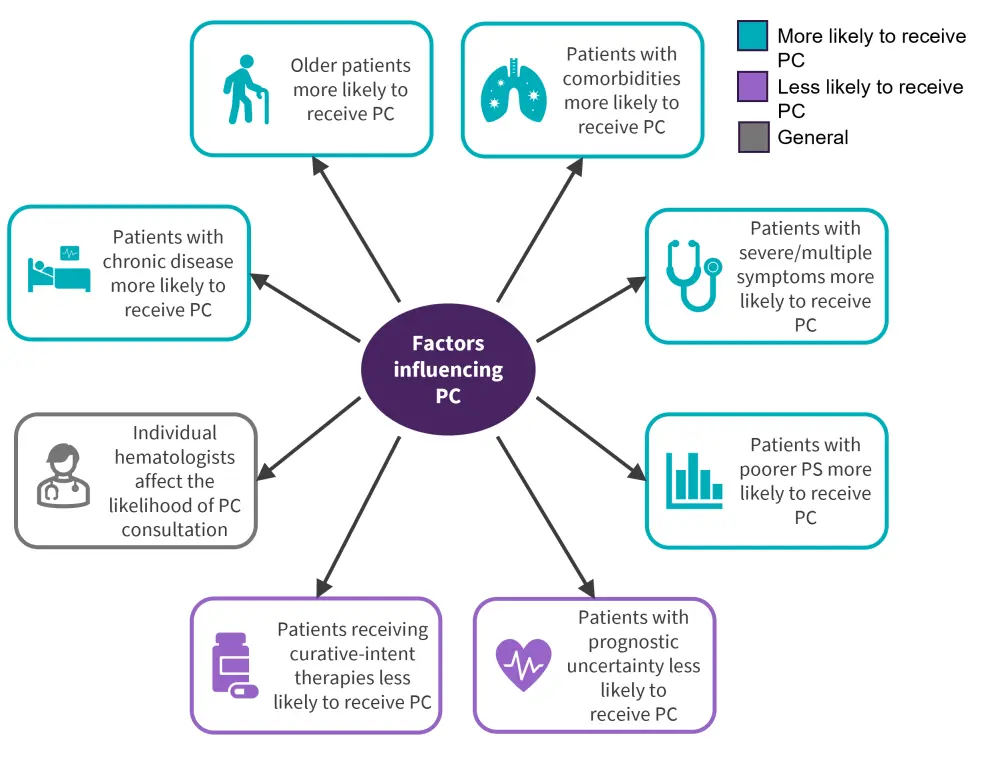
PC, palliative care; PS, performance status.
*Adapted from Santivasi, et al.3
Key findings
- Patient knowledge of what palliative care is increased after a palliative care consultation. Prior to a palliative care consultation, 28% of patients reported having “good” or “excellent” knowledge of palliative care. After a consultation, 78% of patients reported having “good” or “excellent” knowledge of palliative care (13 out of 32 patients said “good” and 12 out of 32 patients said “excellent”).1
- After a consultation, patients feel more comfortable about palliative medicine and are more likely to continue to use it during transplant.1
- As Figure 3 shows, patients who have not had experience with palliative care could benefit from receiving it to help them manage symptoms and to feel that they are part of the decision-making process of their care. However, stigma around palliative care may have prevented them from utilizing it in the past.2
- Figure 4 highlights that palliative care physicians may not always feeling comfortable discussing prognosis with their patients, with some suggesting a multidisciplinary approach involving hematologists would be favorable.3
- There are many factors that may affect a patient’s ability to access palliative care, meaning some patients may not be benefiting from treatment that could improve their quality of life during transplant. Patients with uncertain prognosis are less likely to be offered palliative care than patients with an end-of-life prognosis.3
Conclusion
As shown in these three studies, patient and physician perceptions of what palliative care can offer may differ. Transplant patients with no direct experience with palliative care may not understand what it can offer in terms of symptom management and advance care planning. However, as patients are more likely to utilize palliative care during their transplant after receiving a consultation, increasing knowledge of palliative care in patients undergoing transplant may result in a wider uptake. Ending the stigma around palliative care and improving the relationship between healthcare professionals and their patients could also mean more patients becoming accepting of palliative care. In addition, the quality of palliative care consultations could be improved by increasing physician comfort in explaining diagnoses; this could be done by increasing clinical experience with HSCT and promoting relationships between palliative care physicians and hematologists.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

