All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know ALL.
The all Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the all Hub cannot guarantee the accuracy of translated content. The all and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The ALL Hub is an independent medical education platform, sponsored by Amgen, Autolus, Jazz Pharmaceuticals, and Pfizer and supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View ALL content recommended for you
MRD status as a predictor of survival outcomes in patients with ALL undergoing allo-HSCT in CR2 or later
In patients with acute lymphoblastic leukemia (ALL), measurable residual disease (MRD) status has been demonstrated as a useful predictor of survival outcomes.1 Currently, the American Society for Transplantation and Cellular Therapy (ASTCT) guidelines recommend that allogeneic hematopoietic stem cell transplant (allo-HSCT) is carried out in patients with high-risk ALL within the first complete remission (CR); however, for some patients, allo-HSCT may be deferred to a later stage despite the challenges of maintaining a second CR with allo-HSCT consolidation. The ALL Hub has previously reported an expert opinion on how MRD can guide therapeutic decisions in ALL. Here, we summarize a recent article by Pasvolsky et al.1 examining the prognostic significance of MRD status in patients with ALL undergoing allo-HSCT later than first CR, recently published in Am J Hematol.
Study design
This study enrolled 162 adult and pediatric patients with ALL (B-cell ALL, n = 123; T-cell ALL, n = 39) who underwent allo-HSCT in second CR or later between 2004 and 2021 at the MD Anderson Cancer Center, US. The primary endpoint was cumulative incidence of leukemia relapse, with secondary endpoints including overall survival (OS), progression-free survival (PFS), and non-relapse mortality. Patients were evaluated for their MRD status pretransplant.
Results
Baseline patient characteristics at time of transplant are shown in Table 1.
Table 1. Baseline patient characteristics*
|
Characteristic, % (unless |
Total |
MRD negative |
MRD positive |
p value |
|
B-ALL, B-cell acute lymphoblastic leukemia; CBT, cord blood transplant; CR2, second complete remission; CR3, third complete remission; MRD, measurable residual disease; T-ALL, T-cell acute lymphoblastic leukemia. |
||||
|
Sex |
|
|
|
0.3 |
|
Male |
65 |
67 |
58 |
|
|
Female |
35 |
33 |
42 |
|
|
Median age at transplant, |
31 |
31 |
32 |
0.8 |
|
Diagnosis |
|
|
|
0.4 |
|
B-ALL |
76 |
78 |
72 |
|
|
T-ALL |
24 |
21 |
28 |
|
|
Remission status |
|
|
|
0.02 |
|
CR2 |
80 |
84 |
67 |
|
|
CR3 |
20 |
16 |
33 |
|
|
Graft source |
|
|
|
0.4 |
|
Matched unrelated |
43 |
46 |
35 |
|
|
Matched related |
24 |
23 |
26 |
|
|
Haploidentical |
18 |
18 |
16 |
|
|
CBT |
15 |
13 |
23 |
|
Median follow-up was 51 months in patients who survived (n = 74). Differences in PFS and OS for MRD-positive and MRD-negative patients are shown in Figure 1.
Figure 1. Outcomes in the surviving patients*
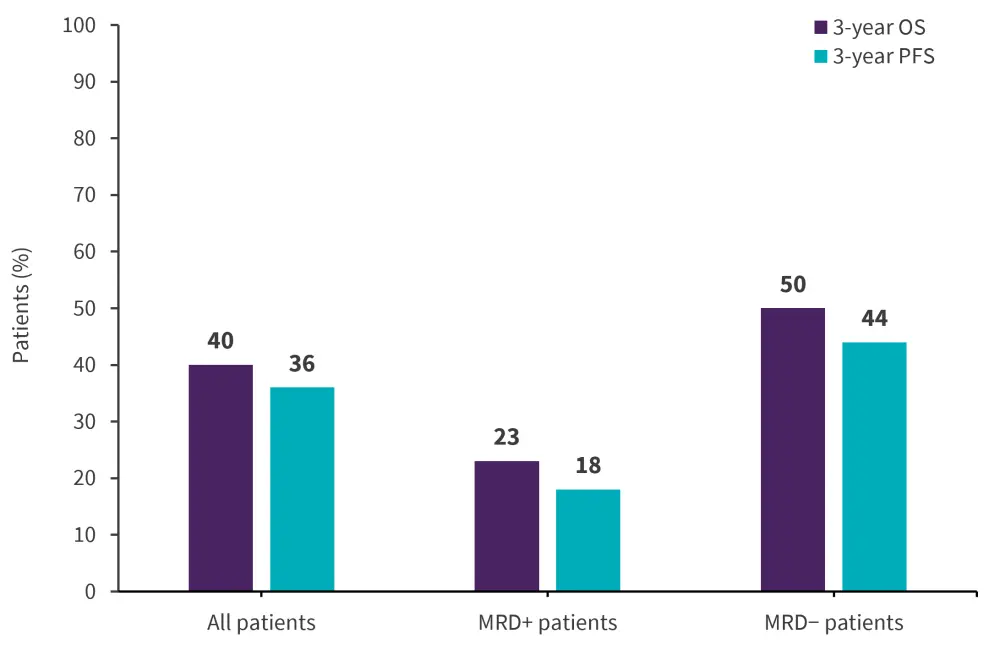
MRD, measurable residual disease; OS, overall survival; PFS, progression-free survival.
*Adapted from Pasvolsky, et al.1
A total of 88 patients died during the study and the primary cause was leukemia progression; causes of death are reported in Table 2. Leukemia progression affected a higher proportion of MRD-positive patients compared with MRD-negative patients.
Table 2. Causes of death*
|
ARDS, acute respiratory distress syndrome; CMV, cytomegalovirus; GvHD, graft-versus-host disease; MRD, measurable residual disease; TA-TMA, transplant-associated thrombotic microangiopathy. |
||
|
Cause of death, % |
MRD negative |
MRD positive |
|---|---|---|
|
Leukemia progression |
55 |
71 |
|
GvHD |
|
|
|
Acute |
11 |
9 |
|
Chronic |
6 |
6 |
|
Infection |
|
|
|
Bacterial |
2 |
0 |
|
CMV |
2 |
3 |
|
Viral/other |
2 |
3 |
|
Infection/other |
2 |
0 |
|
ARDS/ pulmonary failure |
8 |
3 |
|
Liver failure |
8 |
3 |
|
Cardiac failure |
2 |
0 |
|
Secondary malignancy |
2 |
0 |
|
TA-TMA |
2 |
3 |
Impact of MRD status on disease progression
In univariate analysis, pretransplant MRD positivity was associated with reduced OS and an increased relapse rate; ≥2 prior lines of therapy and any conditioning regimen other than total body irradiation was also associated with an increased risk of relapse. Patients who received a transplant in third CR or later had a significantly increased risk of non-relapse mortality and worse OS.
Multivariate analysis showed a similar association between pretransplant MRD positivity and increased rate of relapse, reduced OS, and worse PFS. In patients who received a transplant in their third CR or beyond, MRD status was not found to be associated with relapse risk.
Conclusion
This study demonstrated that in patients with ALL undergoing allo-HSCT in second CR or beyond, pretransplant MRD positivity is a key predictor of disease relapse, PFS, and OS.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


