All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know ALL.
The all Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the all Hub cannot guarantee the accuracy of translated content. The all and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The ALL Hub is an independent medical education platform, sponsored by Amgen, Autolus, Jazz Pharmaceuticals, and Pfizer and supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View ALL content recommended for you
Ponatinib and venetoclax for patients with Philadelphia chromosome-positive ALL: Interim results of a phase I/II study
The third-generation, pan–BCR-ABL tyrosine kinase inhibitor (TKI), ponatinib, is effective for treating patients with Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL) who are not eligible for other TKIs, such as dasatinib, or present with a T315I mutation. However, the effect is not durable, with a reported 1-year progression free survival (PFS) of only 8%.1 As ALL cells are highly dependent on Bcl-2 for survival, inhibitor venetoclax is a promising candidate for treatment. The hypothesis is that venetoclax and ponatinib may act synergistically in Ph+ ALL by inhibiting LYN tyrosine kinase and blocking Mcl-1 upregulation.
At the 62nd American Society of Hematology (ASH) Annual Meeting and Exposition, Nicholas Short presented the interim results of a phase I/II trial (NCT03576547) of ponatinib, venetoclax, and dexamethasone in patients with Ph+ ALL.1
Study design
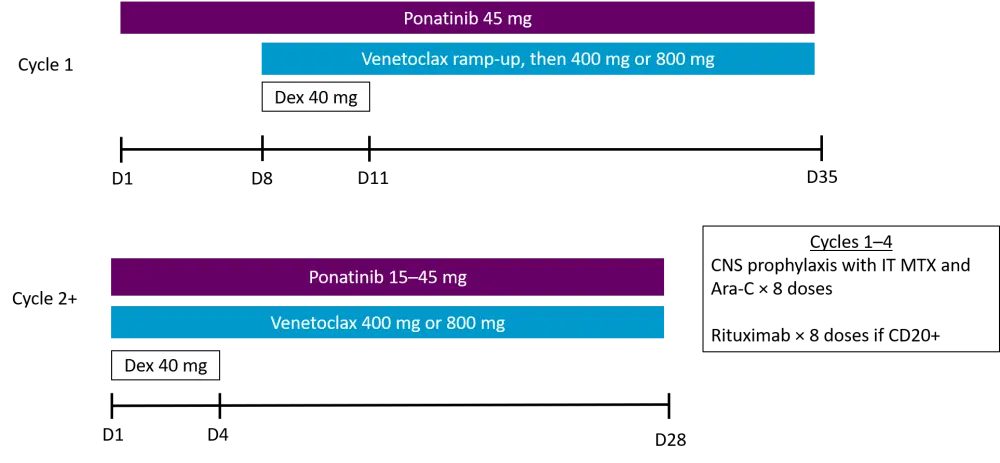
In Cycle 1, patients that had not received ponatinib in the last 2 weeks received 7 days of ponatinib monotherapy at 45 mg daily. On Days 8−11, ponatinib was given with venetoclax and dexamethasone as shown in Figure 1. Venetoclax was ramped up in Cycle 1 to 400 mg for dose level 1 and 800 mg for dose level 2. In Cycle 2 and subsequent cycles, ponatinib was decreased daily down to 30 mg if patients reached complete response (CR)/CR with incomplete hematological recovery (CRi) or to 15 mg if patients were in complete metabolic response (CMR). Central nervous system prophylaxis was given during Cycles 1−4, and rituximab was added if blast cells were CD20 positive.
Figure 1. Study design1
Primary endpoints:
- Phase I: maximum tolerated dose of venetoclax combination
- Phase II: CR/CRi rate
Secondary endpoints:
- CMR rate
- Relapse-free survival (RFS)
- Overall survival (OS)
- Safety
Eligibility
Eligible patients were ≥ 18 years of age and diagnosed with relapsed/refractory Ph+ ALL or chronic myeloid leukemia in the lymphoid blast phase that had been treated with at least one tyrosine kinase inhibitor. Patients were required to have adequate hepatic and renal function, no uncontrolled active cardiovascular disease, and no previous exposure to venetoclax.
Patient characteristics
Patient characteristics are detailed in Table 1, which shows a young population with a median age of 37 years, who had received a median of three previous therapies. Half of the patients were positive for the T315I mutation and, not surprisingly, many had been treated with ponatinib before (78%). In addition, two thirds had undergone stem cell transplantation.
Table 1. Patient baseline characteristics of nine patients enrolled1
|
CNS, central nervous system; HSCT, hematopoietic stem cell transplant; TKI, tyrosine kinase inhibitor; WBC, white blood cell. |
||
|
Characteristic |
Category |
Median, % unless stated otherwise |
|---|---|---|
|
Age, years (range) |
|
37 (26−73) |
|
Performance status |
0−1 |
89 |
|
|
2 |
11 |
|
WBC, × 109/L (range) |
|
5.2 (0.2−8.9) |
|
CNS/extramedullary involvement |
|
33 |
|
BCR-ABL1 transcript type |
p190 |
89 |
|
|
p210 |
11 |
|
T315I mutation |
|
50 |
|
No. prior therapies (range) |
|
3 (2−4) |
|
No. of prior TKIs (range) |
|
2 (1−3) |
|
Prior ponatinib |
|
78 |
|
Prior blinatumomab |
|
56 |
|
Prior HSCT |
|
67 |
|
Venetoclax dose |
400 mg |
33 |
|
|
800 mg |
67 |
Safety
Regarding the safety profile, no dose limiting toxicities were observed and no early mortality was seen. So far, three patients are at 400 mg (dose level 1) in Cycle 1 and six are at 800 mg (dose level 2). The adverse events are shown in Table 2. Most events recorded were low grade, with only two cases of Grade 4 neutropenia and one Grade 4 thrombocytopenia. Neutropenia was the most common event, occurring in three cases. 800 mg venetoclax has been selected as the recommended phase II dose.
Table 2. Adverse events1
|
ALT, alanine transaminase; AST, aspartate aminotransferase; GI, gastrointestinal; UTI, urinary tract infection. |
|||
|
Adverse events in 9 patients |
All grade, n |
Grade 3, n |
Grade 4, n |
|---|---|---|---|
|
ALT increased |
3 |
3 |
0 |
|
Febrile neutropenia |
3 |
3 |
0 |
|
Neutropenia |
3 |
1 |
2 |
|
Alkaline phosphatase increased |
2 |
1 |
0 |
|
AST increased |
2 |
0 |
0 |
|
Thrombocytopenia |
2 |
0 |
1 |
|
Pain |
2 |
2 |
0 |
|
GI hemorrhage |
1 |
1 |
0 |
|
Pneumonia |
1 |
1 |
0 |
|
Altered mental status |
1 |
1 |
0 |
|
Thromboembolic event |
1 |
1 |
0 |
|
UTI |
1 |
1 |
0 |
|
Lower extremity weakness |
1 |
1 |
0 |
In this trial, the median number of cycles received was three (range, 1−12). Dose reductions occurred in five patients:
- Ponatinib in four cases (transaminase elevation, n = 3; possible transient ischemic attack/peripheral sensory neuropathy, n = 1)
- Venetoclax in one case due to myelosuppression
Dose interruptions occurred in five patients:
- Ponatinib in five cases (transaminase elevation, n = 3; myelosuppression, n = 1; deep vein thrombosis/pulmonary embolism, n = 1)
- Venetoclax in four cases as a result of myelosuppression
Efficacy
Patient responses are shown in Table 3. All but one patient responded after one cycle of treatment. The one non-responding patient had extramedullary disease and responded after two cycles. In one patient, bone marrow blasts reduced from 94% to 6% with almost full neutrophil and platelet recovery but did not meet complete response criteria.
Among the five responding patients, all but one also achieved CMR. The CR patient who did not achieve CMR had only completed one cycle. Of the four patients achieving CMR, three did so after one cycle.
Table 3. Response to ponatinib and venetoclax1
|
CMR, complete metabolic response; CR, complete response; CRi, CR with incomplete hematological recovery. |
|
|
Response |
N = 9 |
|---|---|
|
CR/CRi |
5 |
|
CR |
4 |
|
CRi |
1 |
|
CMR |
4 |
|
CMR after Cycle 1 |
3 |
The median follow-up in nine patients was 10.8 months (range, 1.0–13.2), and the estimated 1-year OS for ponatinib and venetoclax was 63%. Further subanalysis demonstrated:
- All four patients in dose level 1 receiving venetoclax at 400 mg/day did not respond
- Five of six patients in dose level 2 (800 mg/day of venetoclax) achieved CR/CRi and none have relapsed so far, giving a 6-month RFS of 100%
- Out of these, four remain on study in remission, and one patient due to deep vein thrombosis/pulmonary embolism was taken off study (still in remission on a combination of bosutinib and venetoclax)
Conclusion
In this heavily pretreated population of patients with relapsed/refractory Ph+ ALL the combination of ponatinib and venetoclax appeared safe and effective with a 100% RFS at 6 months, which compares favorably with ponatinib monotherapy. Improved results, and no dose-limiting toxicity, have been demonstrated in the subgroup treated with 800 mg/day of venetoclax, which has now been taken forward as the recommended dose for the ongoing phase II part of the study.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

