All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know ALL.
The all Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the all Hub cannot guarantee the accuracy of translated content. The all and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The ALL Hub is an independent medical education platform, sponsored by Amgen, Autolus, Jazz Pharmaceuticals, and Pfizer and supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View ALL content recommended for you
Novel treatment approaches in Ph+ ALL: Key updates from EHA 2023
Historically, Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL) has been associated with poor prognosis; however, the advent of monoclonal antibodies and tyrosine kinase inhibitors (TKIs), particularly third-generation TKIs, have demonstrated promising activity against several BCR-ABL mutations, significantly improving the treatment landscape for this patient subset.1
The ALL Hub previously reported on novel treatment approaches in Ph+ ALL. Here, we provide further updates on novel treatment regimens for adult patients with Ph+ ALL, highlighting five key trials presented by Nicholas Short,2 Kaibo Zhu,3 Weiyang Liu,4 Fadi Haddad,5 and Heike Pfeifer6 at the European Hematology Association (EHA) 2023 Congress.
Ponatinib plus blinatumomab in newly diagnosed Ph+ ALL: subgroup analysis from a phase II study2
This is an ongoing phase II substudy of ponatinib plus blinatumomab in newly diagnosed adult patients with Philadelphia chromosome-positive (Ph+) ALL (NCT03263572). This trial included patients aged ≥18 years, with newly diagnosed Ph+ ALL, an ECOG Performance Status of 0–2, and adequate hepatic function. The treatment schedule was previously described, here. The primary endpoint was complete molecular response (CMR) rate and secondary endpoints included event-free survival, overall survival, and safety.
In total, 60 patients were treated with the ponatinib and blinatumomab combination. Baseline characteristics were similar to that previously reported, with a median age of 55 years and 57% of patients having ≥1 cardiovascular risk factor.
Efficacy
Response rates among the 60 evaluable patients in the newly diagnosed cohort are reported in Table 1. After cycle one, paired minimal residual disease (MRD) samples showed that the majority of patients achieving MRD negativity by polymerase chain reaction (PCR) were MRD positive by next-generation sequencing (NGS). There was concordance between PCR and NGS MRD response overall, though there was discordance in 20% of patients.
Table 1. Efficacy outcomes*
|
ALL, acute lymphoblastic leukemia; CR, complete response, CRi, complete response with incomplete hematologic recovery; EFS, event-free survival; MRD, minimal residual disease; NGS, next-generation sequencing; ORR, overall response rate; OS, overall survival; Ph, Philadelphia chromosome. |
|
|
Response, % |
Newly diagnosed Ph+ ALL (n = 60) |
|---|---|
|
Hematologic responses† |
|
|
ORR |
97 |
|
CR |
95 |
|
CRi |
3 |
|
Early death |
3 |
|
Complete molecular response‡ |
|
|
Overall |
83 |
|
After cycle one |
67 |
|
NGS MRD negative |
89 |
|
After cycle one |
45 |
|
Survival analysis |
|
|
2-year EFS |
79 |
|
2-year OS |
88 |
Safety
- There was only one Grade 4 ponatinib-related adverse event (AE) of increased lipase reported.
- Ponatinib related Grade 3 AEs included increased alanine transaminase (n = 6); increased lipase (n = 3); pancreatitis (n = 2); and rash, hypertension, atrial fibrillation, and coronary artery stenosis in one patient each.
- There were no Grade 3 or higher AE’s related to blinatumomab, all AE’s were grade 1-2.
- Overall, four deaths were reported, two in complete response (CR), one early death and one in relapse
Presenter’s conclusion
The chemotherapy-free combination of ponatinib plus blinatumomab induces deep, early, rapid, and durable remissions without the need for hematopoietic stem cell transplantation (HSCT) in first remission for newly diagnosed adult patients with Ph+ ALL. The protocol has been amended to increase the number of intrathecal prophylaxis doses to mitigate CNS relapses.
Olverembatinib plus PDT-ALL 2016 protocol in newly diagnosed Ph+ ALL3
The efficacy and safety results of olverembatinib combined with PDT-ALL 2016, a pediatric inspired chemotherapy, in adults aged 16−64 with newly diagnosed Ph+ ALL in China were presented by Zhu. Patients received ≤3 courses of chemotherapy according to the PDT-ALL 2016 protocol combined with oral olverembatinib at 40 mg once every other day. The study endpoint was CMR, defined as the absence of a detectable BCR-ABL1 transcript by real-time PCR at a sensitivity level of 10−2.
Efficacy and safety
In total, 13 patients were enrolled and treated with this combination. At a median follow-up of 8.967 months,
- all patients achieved CR;
- median overall survival (OS) was not reached;
- a higher CMR was observed following each assessed timepoint at Day 14, 30, 60, and 90, respectively (Figure 1); and
- three patients experienced AE’s including two patients with skin pigmentation and one with hypertension.
Figure 1. Response rates*
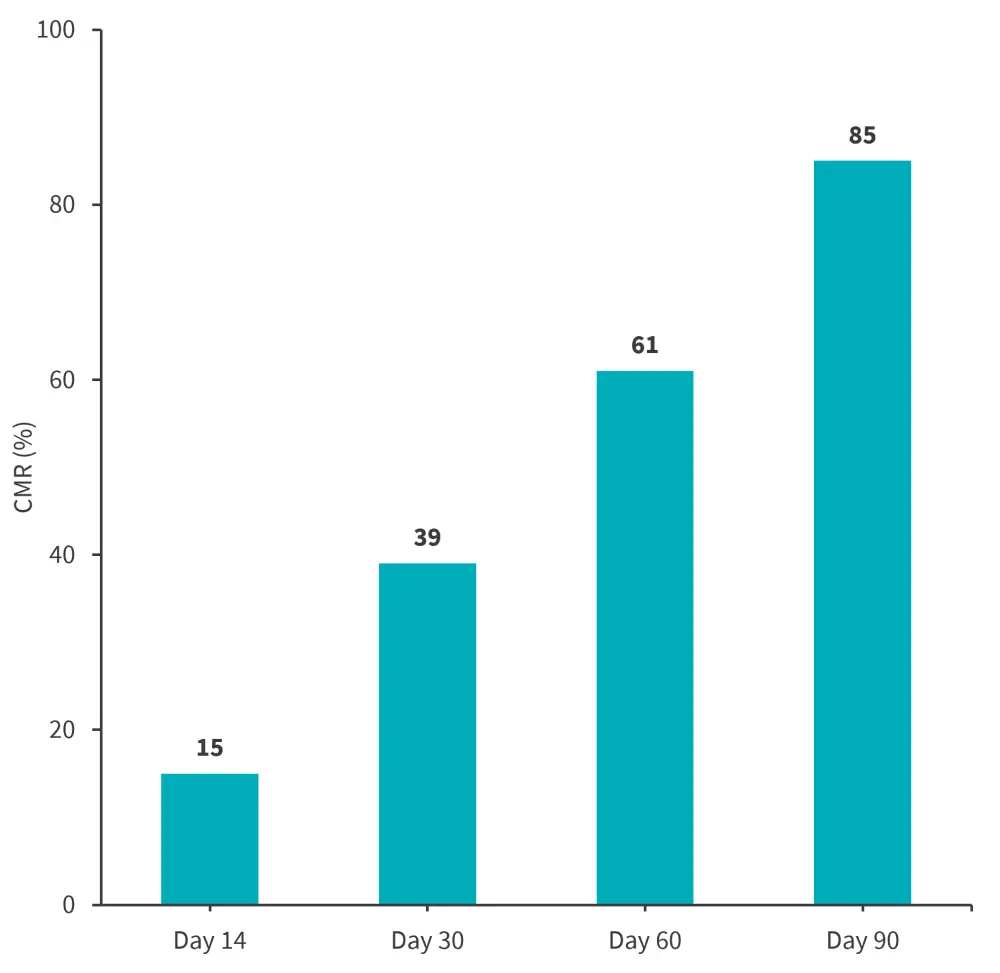
CMR, complete molecular response.
*Data from Zhu et al3
Presenter’s conclusion
Olverembatinib combined with PDT-ALL 2016 demonstrated promising efficacy and an acceptable safety profile in newly diagnosed adult patients with Ph+ ALL; therefore, this remains a promising frontline standard-of-care approach for this patient subset, though further study is needed.
Olverembatinib in adults with Ph+ ALL harboring T315I mutation and relapsed/refractory disease4
The updated results of olverembatinib in adult patients with relapsed/refractory (R/R) Ph+ ALL harboring the T315L mutation in China were presented by Liu. Patients received olverembatinib monotherapy at 40 mg every 2 days or in combination with vincristine/prednisone-based low-intensity chemotherapy. Efficacy endpoints included CR rate, MRD negativity rates by multicolor flow cytometry, CMR, progression-free survival (PFS), and OS. Safety endpoints were AEs according to the common terminology criteria for adverse events v5.0.
Efficacy
Of the 21 patients treated with olverembatinib, the median age was 60 years. Overall, 11 patients were in CR with molecular R/R disease and the remaining 10 had hematological R/R disease.
- Among the entire cohort, the overall response rate, MRD-negativity, and CMR rates were 71%, 62%, and 52%, respectively.
- Among the 11 patients with molecular R/R disease, MRD-negativity and CMR were 73% and 64%, respectively.
- Among the 10 patients with hematological R/R disease, the CR, MRD-negativity, and CMR were 70%, 50%, and 40%, respectively.
- CMR and MRD rates were significantly higher in patients with vs without the T315l mutation (Figure 2).
- At a median follow-up of 6 months, PFS and OS rates were 52% and 65%, with higher PFS and OS amongst CMR and MRD-negative responders.
- Of treated patients, 11 had durable remissions and remained in CMR or MRD-negativity, four had no response or disease relapse, and there were six deaths due to disease relapse.
Figure 2. CMR and MRD rates in T315lmut versus T315lwt*
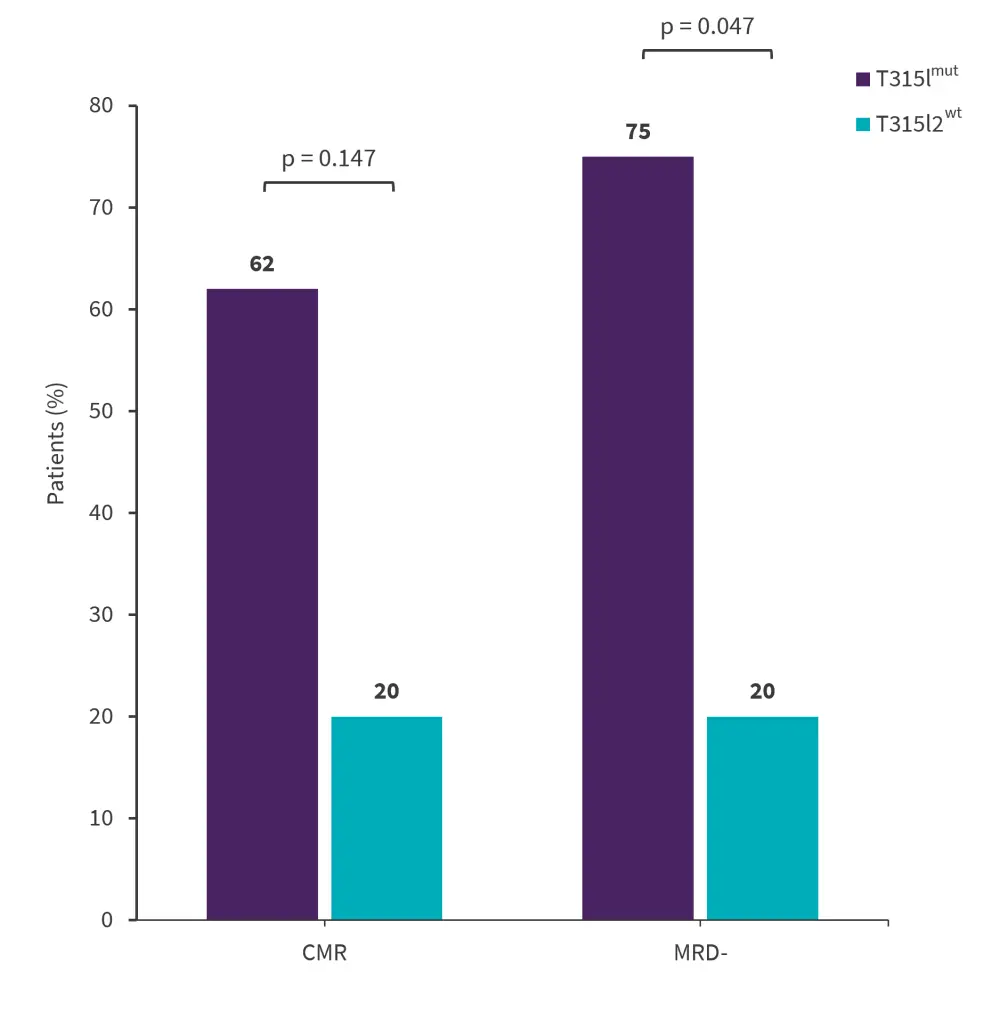
CMR, complete molecular response; MRD, minimal residual disease.
*Data from Liu.4
Safety
All patients experienced at least one treatment-related AE. Non-hematological AE’s were mostly Grade 1 or 2 and hematological AE’s were mostly Grade 3 or 4. No deaths related to olverembatinib were reported.
Presenter’s conclusion
Overall, olverembatinib proved effective and well-tolerated in Chinese adult patients harboring the T315L mutation with molecular or hematological R/R disease.
Mini hyperfractionated cyclophosphamide, vincristine, and dexamethasone and ponatinib followed by blinatumomab and ponatinib in Ph+ ALL: a phase II study5
Data from a phase II study on mini hyperfractionated cyclophosphamide, vincristine, and dexamethasone mini-hyper-CVD and ponatinib followed by blinatumomab and ponatinib in adult patients with newly diagnosed Ph+ ALL, R/R Ph+ ALL, and chromic myeloid leukemia in lymphoid blast phase (CML-LBP) were presented by Haddad. The primary endpoints were CMR in the newly diagnosed cohort, and CR/CRi rates in the CML-LBP and R/R cohorts. Secondary endpoints included CR duration, overall survival, and safety.
Results
All treated patients (n = 17) achieved a CR; response rates are summarized in Figure 3. The 2-year remission durations in the total and newly diagnosed cohorts were 92% and 89%, respectively. The 2-year OS for both the total and newly diagnosed cohorts was 81%. Relapse rates were low, with only one case reported among the newly diagnosed cohort.
Figure 3. Responses*
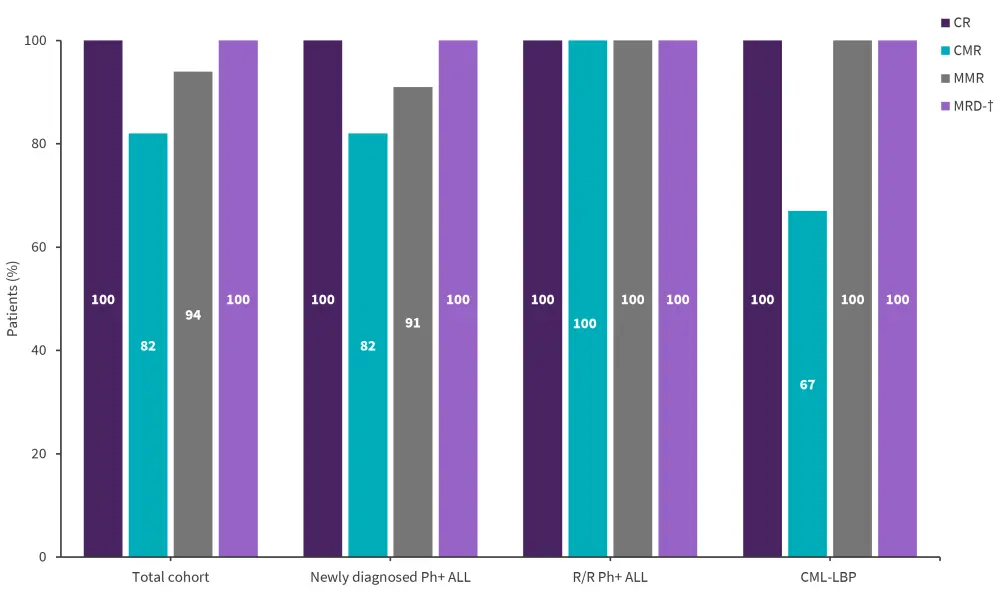
ALL, acute lymphoblastic leukemia; CML-LBP, chronic myeloid leukemia-lymphoid blast phase; CMR, complete molecular response; CR, complete response; MMR, major molecular response; MRD, minimal residual disease; Ph, philadelphia chromosome.
*Data from Haddad.5
†Seven patients across the three cohorts were evaluable for MRD, five in the newly diagnosed and one each in the R/R and CML-LBP cohort.
Safety
Overall, treatment was well-tolerated. Ponatinib dose was reduced in two patients due to toxicity and there was one ponatinib discontinuation due to pulmonary embolism. There were no blinatumomab dose reductions or discontinuations, with no deaths reported on Day 60 and 90.
Presenter’s conclusion
The sequential combination of mini-hyper-CVD and ponatinib followed by blinatumomab and ponatinib proved effective and well-tolerated in patients with Ph+ ALL and CML-LBP.
Imatinib combined with dose-reduced induction followed by stem cell transplantation in Ph+ ALL: GMALL trial 08/136
Outcomes from the phase IV GMALL 08/13 trial (NCT02881086) evaluating dose-reduced induction combined with imatinib followed by stem cell transplantation in patients with Ph+ ALL were presented by Pfeifer. MRD was assessed by quantitative reverse transcriptase PCR at different timepoints, with additional MRD analyses by immunoreceptor gene/T cell receptor quantitative reverse PCR.
Efficacy
Overall, 165 patients with a median age of 42 years were treated. A high proportion of patients achieved hematologic remissions, with CR rates of 85%, 95%, and 93% after induction I, induction II and consolidation II, respectively. Low mortality was also observed, with early death and failure rates of 5% and 1%, respectively. The CMR after induction I, induction II, and consolidation I are reported in Figure 4. Among the total cohort, the 3-year OS and remission duration rates were 74% and 89%, respectively; the 3-year OS rate for patients receiving SCT was 79%.
Figure 4. Molecular responses*
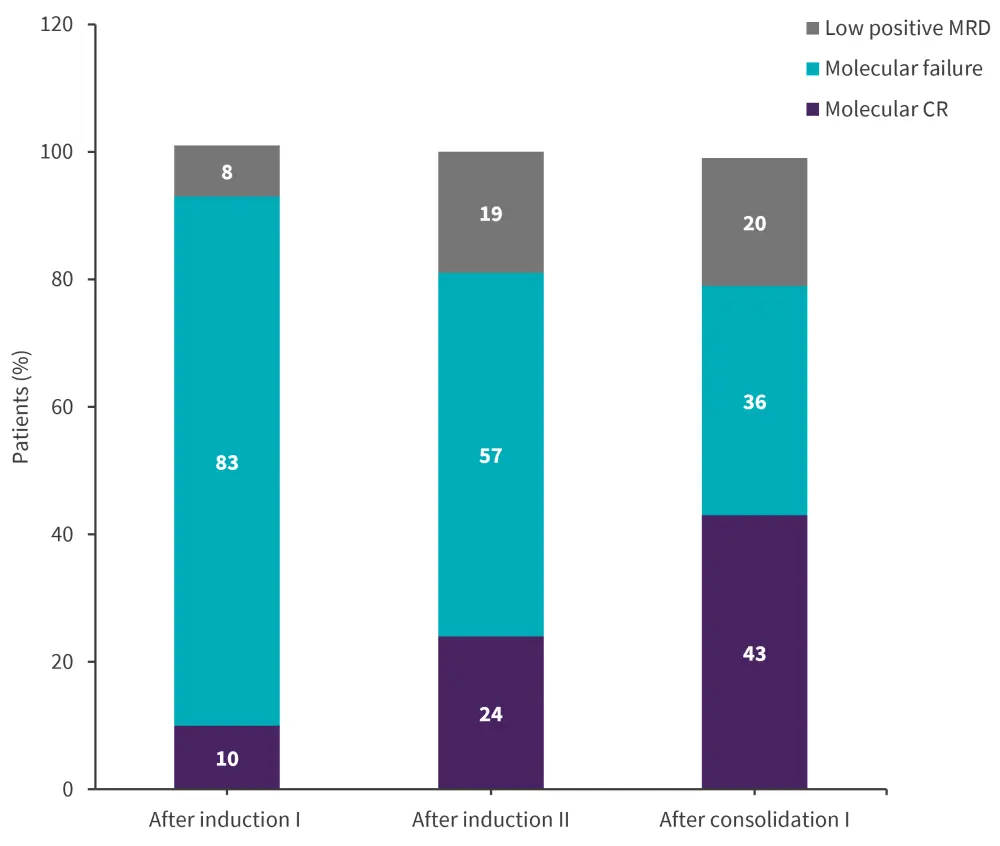
CR, complete response; MRD, minimal residual disease.
*Data from Pfeifer.6
Presenter’s conclusion
Low intensity chemotherapy combined with imatinib yielded high responses and low mortality rates in adult patients with Ph+ ALL, therefore, this remains a promising treatment regimen, though longer follow-up results after stem cell transplantation warranted. Future trials should investigate the prognostic role of BCR:ABL1 MRD in transplant-focused regimens; the upcoming GMALL EVOLVE trial will evaluate the use of TKIs and immunotherapies in this patient population with the aim of reducing the need for SCT.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content




