All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit Know ALL.
The all Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the all Hub cannot guarantee the accuracy of translated content. The all and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The ALL Hub is an independent medical education platform, sponsored by Amgen, Autolus, Jazz Pharmaceuticals, and Pfizer and supported through an educational grant from the Hippocrate Conference Institute, an association of the Servier Group. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View ALL content recommended for you
Blinatumomab in infants with KMT2A-rearranged ALL
Infants (<1-year-old) with acute lymphoblastic leukemia (ALL) have worse survival outcomes than older children, this is further pronounced with the presence of a KMT2A rearrangement (KMT2Ar). KMT2Ar is common in infant patients (75%) and produces high rates of early relapse, it is therefore associated with reduced survival (20%).
Blinatumomab is an anti-CD19 bispecific T-cell engager that has previously demonstrated efficacy and safety in both older children and adult patients with ALL. In the Interfant-06 trial (NCT00550992), the largest clinical trial in infants with ALL to date, the 6-year event-free survival rate was 36% and most relapses occurred during the first 2 years.1 The ALL hub has previously reported outcomes from the addition of blinatumomab to the Interfant-06 study protocol in infants with newly diagnosed ALL. Here, we summarize a recent publication by van der Sluis et al.1 in New England Journal of Medicine evaluating the safety and efficacy of blinatumomab added to the interfant-06 backbone regimen in infants with KMT2A-rearranged ALL.
Study design1
This was a phase II, prospective, multicenter study including patients aged <1 year. Patients with newly diagnosed KMT2A-rearranged, CD19+, B-precursor ALL, with <25% leukemic blasts in their bone marrow at the end of the induction were included and treated according to the Interfant-06 protocol. Patients with clinically relevant central nervous system (CNS) conditions requiring additional treatment or evidence of CNS involvement at the end of induction were excluded. Following blinatumomab infusion, treatment was continued in line with the Interfant-06 protocol (Figure 1).
Figure 1. Treatment protocol of theInterfant-06 trial with the addition of blinatumomab therapy*
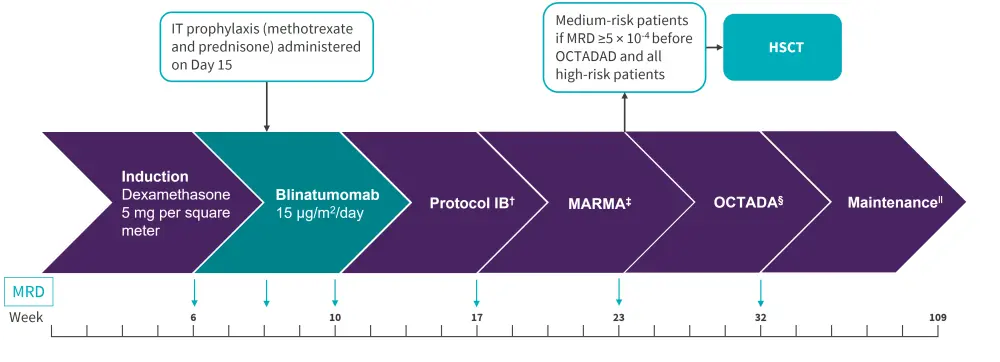
IT, intrathecal; HSCT, hematopoietic stem cell transplant; MRD, minimal residual disease.
*Adapted from van der Sluis, et al.1
†Consisted of cyclophosphamide, cytarabine, and mercaptopurine.
‡Consistsed of high dose cytarabine, high dose methotrexate, mercaptopurine, and asparaginase. §Consisted of vincristine, dexamethasone, asparaginase, daunorubicin, thioguanine, cytarabine, and cyclophosphamide.
‖Consisted of mercaptopurine and methotrexate.
The primary endpoint was clinically relevant toxic effects, classified as any toxic effect that was possibly or definitely related to blinatumomab that resulted in blinatumomab discontinuation or death. Secondary endpoints were toxicity (including serious adverse events [AEs] according to Common Terminology Criteria for Adverse Events version 4.03), the number of treatment interruptions, and the percentage of patients receiving the full 4 week course of blinatumomab. Data on AEs were gathered at the start of blinatumomab infusion until the start of protocol IB, with these findings then compared with historical control data from the Interfant-06 trial. Additional secondary efficacy endpoints included minimal residual disease (MRD) response, percentage of medium-risk patients with MRD of at least 5 × 10−4 before OCTADAD treatment, and long-term outcomes.
Results1
In total, 30 patients were treated and included in this study analysis. There was no significant difference in baseline characteristics between patients in this study versus the Interfant-06 trial historical cohort. In total, eight out of nine high-risk patients successfully received hematopoietic stem cell transplantation (HSCT) in first complete remission, with none of the medium-risk patients achieving the required MRD levels prior to OCTADAD for HSCT.
Adverse events
No toxic effects related to blinatumomab, leading to treatment discontinuation, or death were reported. All patients received the full 4-week course of blinatumomab.
In total, 78 AEs of any grade occurred, including ten serious AEs reported in nine patients. The most common Grade 1 or 2 AEs were hypertension, vomiting, and diarrhea (13% each); the most common Grade 3 AEs were anemia, febrile neutropenia, neutropenia, and elevated γ-glutamyl transferase level (Table 1).
Table 1. Adverse events*
|
AE, adverse event; CTCAE, Common Terminology Criteria for Adverse Events *Adapted from van der Sluis, et al.1 ‡Grade 1 fever occurred twice in one patient. |
|
|
Adverse Events, % |
(N = 30) |
|---|---|
|
Serious AEs |
30 |
|
Grade 3 or 4 infection |
13 |
|
Grade 1 fever‡ |
10 |
|
Grade 3 hypertension |
3 |
|
Grade 3 vomiting |
3 |
|
AEs of CTCAE grade ≥3 |
|
|
Anemia |
17 |
|
Febrile neutropenia |
7 |
|
Pharyngitis |
3 |
|
Hypertension |
3 |
MRD response
A total of 28 patients achieved MRD-negativity at the end of blinatumomab treatment.
- At 2 and 4 weeks post-blinatumomab treatment, 53% of patients achieved MRD-negativity.
- MRD negativity at the end of the blinatumomab treatment occurred more frequently among medium-risk vs high-risk patients (67% vs 22%) and among those with low vs high MRD levels at the end of induction (78% vs 17%).
- Out of the 22 patients that were MRD-positive at the end of the induction treatment, nine became MRD-negative following blinatumomab treatment.
The rate of MRD-negativity, or MRD ≤5 × 10−4, in this study population compared with the Interfant-6 study at different time points is shown in Figure 2.
Figure 2. MRD at treatment timepoints throughout the study*
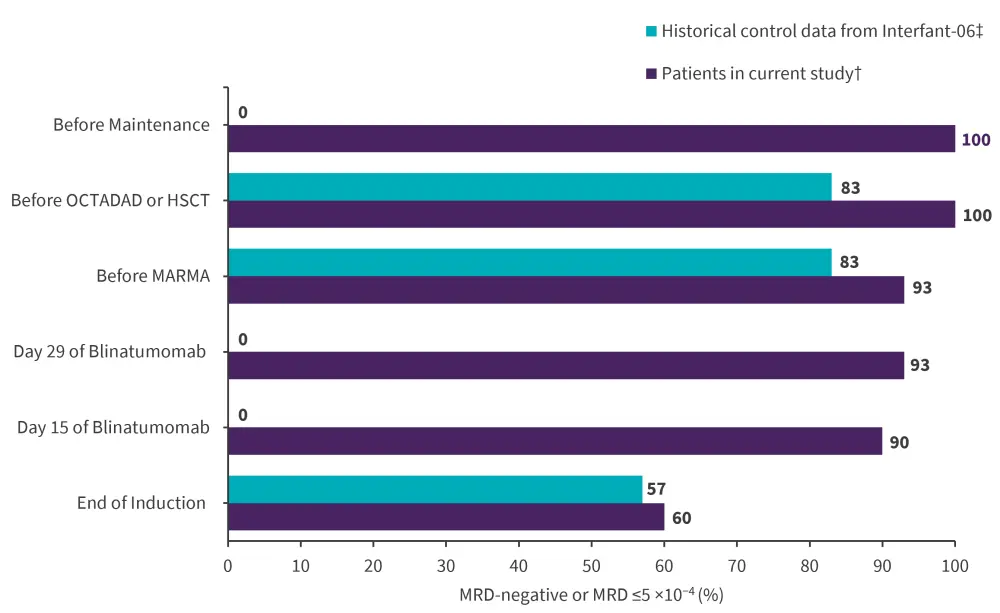
*Adapted from, van der Sluis et al.1
†n = 30.
‡n=284.
Overall and disease-free survival
After a median follow-up of 26.3 months, the 2-year overall and disease-free and survival rates were higher compared with the historical interfant-06 trial (Table 2).
Table 2. Comparison of disease-free survival and overall survival in the Interfant-06 study vs addition of blinatumomab*
|
CI, confidence interval. |
|
|
|
|
With the addition of |
Interfant-06 |
|---|---|---|
|
2-year disease-free survival |
81.6% |
49.4% |
|
2-year overall survival |
93.3% |
65.8% |
Hazard ratios comparing data from both groups of patients in the study versus the historical control data were 0.22 (95% confidence interval [CI], 0.09–0.34) for 2-year disease-free survival and 0.15 (95% CI, 0.04–0.62) for 2-year overall survival.
Conclusion
Addition of fixed-dose blinatumomab to the current standard chemotherapy regimen was found to be effective, with a manageable safety profile in infants with newly diagnosed KMT2A-rearranged ALL. This regimen demonstrated improved rates of MRD-negativity, improved short-term survival, and fewer acute adverse effects compared to standard chemotherapy. Future trials should investigate whether additional courses of blinatumomab can further improve outcomes and the role of HSCT in high-risk patients.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


